It actually covers all costs relating to dental health and care. Dental health is also referred to as oral health, and it may be important to one’s general health; therefore, people take it as part of their health insurance. In most cases, dental insurance can also be included under medical insurance health plans or bought separately from a dental insurer, Health Insurance Marketplace, or private broker.
Dental Insurance vs. Dental Benefits
When purchasing insurance, one would probably come across the term “dental benefits,quot which you realise is different from dental insurance.
Insurance really means pooling risk (for example, the risk that you will have to pull a tooth out or get a root canal and pay out costs accordingly).
Some things are fully covered under a benefits plan, and others specific things only partially, and others are not at all. It should be useful but not one-size-fits-all.
Do you have dental benefits? Have you read the fine print to find out what type would be best for you?
NADP reports that over 79% of Americans have some dental benefits. Most have the private indemnity form usually provided by the employer or group programs. Large employers are more likely to provide dental benefits compared to small employers. High-wage employees tend to have higher chances of getting dental benefits than low-wage employees. Medicare never pays for dental services, and most state Medicaid programs pay for dental care to children exclusively.

You have to know these things so that you can maximize your benefits. While shopping for a dental coverage plan, ensure that you understand the type of plan that you opt for and the coverage it provides.
Dental Insurance Categories
Although plans can be different from each other in a lot of respects, the most common types of dental insurance are described below:
Direct reimbursement program
In direct reimbursement programs, you would get a specified percentage of your total expenses for dental care, irrespective of what kind of treatment it is. Generally, this model does not exclude coverage based on the type of treatment needed and would grant you the freedom to choose any dear dentist. Moreover, it makes both work with your dentist to look for health and economically sound solutions.
Programs for “Usual, Customary, and Reasonable” (UCR).
Usual, Customary and Reasonable, U-CR programs allow a patient to avail themselves of any type of dentist. These plans pay a predetermined percentage of the dentist’s fee or the plan administrator’s “reasonable” or “customary” fee limit, whichever is lower. The objective of these boundaries is to be tied to a contract entered into between the plan purchaser and the third-party payer. Though these ceilings are called “customary,” they can or cannot accurately represent the usual charges among dentists in the locality. There is a wide variation and a lack of government regulation with regard to plans on how a “customary” fee level for that plan is determined.
Table or schedule of allowance programs
These are written programs that have covered services in dollar amounts suggested as amounts that the plan will pay for services it covers without regard to the fee charged by the dentist. The amounts between the allowed charge and the dentist’s fee will then be billed to you, which is called balance billing.
Capitation programs
To capitate contracted dentist payments for several enrolled families or patients, most of the time, dentists will usually know the terms under which they would be contacting patients in treatment free of charge. Some treatments still require co-payments. Although the capitation premium might vary greatly from that which the plan offered for the patient’s actual dental care, it might still differ.
Dental Insurance Program.
The amount of dental insurance is generally much more similar to health insurance in some aspects, and quite different in other ways. The options you will usually find include:
Preferred Provider Organization(PPO)
Like that of health insurance PPOs, a list of dentists as well as other oral health care providers that accept the plans, is included in these plans. These are identified as in-network providers. By going to such a provider, you incur the least out-of-pocket expenses. As an option, going out of network may be available; the payment should be incurred using an in-network provider in general, and such expenses will be relatively lower.
Dental Health Maintenance Organization (DHMO)
Similar to a health insurance HMO, almost all co-pays under the DHMO plans are set aside, rendering a dentist accessible upon accepting the plan fee. You might not be able to consult an outside dentist, as the network restricts its participants. Conforming to that, if you see an outside dentist, you pay for services rendered yourself.
Discount or Referral Dental Plan
When a specific number of dentists participate in such discount referral dental plans, they offer discounts on certain procedures. This, unlike health insurance, pays you absolutely nothing for your treatment. This also works as an access plan or a savings plan.
Private Dental Insurance
In speaking about dental coverage that an individual buys privately, this coverage does not come from an employer. Private insurance can be purchased from a dental insurer, HealthCare.gov, or an insurance broker.
Dental Insurance for Seniors and Low-Income Residents
You have reached the age of 65, or you may be eligible for government programs due to low income and resources. These plans have specific provisions on how they handle dental coverage:
Medicare
People aged 65 years and older are generally insured by Medicare. Some Medicare beneficiaries, however, qualify because they have a disability, amyotrophic lateral sclerosis, or end-stage renal disease. For most employees and employers, as well as for many self-employed individuals, Medicare actually receives most of its funds from payroll taxes. Most people pay no monthly premium for Part A, hospital insurance benefits under Medicare; for Part B, medical insurance benefits under Medicare, you will pay monthly premiums.
Medicare does not normally cover dental services, such as routine cleaning, filling, or extraction, but it does not cover items like dentures. These services are paid for wholly by the patient. Some dental procedures, where you would have to be admitted as an inpatient into a hospital because of the complexity of the dental procedure or because of another medical condition you have, might be covered by Medicare. In addition, certain inpatient and outpatient dental services related to covered medical conditions or to the success of medical treatment may be included in the coverage provisions. This entails an out-of-pocket share to cover the Medicare Part A deductible and co-pays for your hospital stay. For the Part B covered dental services, you pay 20 percent after meeting the deductible for Part B. As for the facility co-payment, you will incur for the entire covered dental services rendered in other outpatient or dentists’ offices.
Medicare Advantage Plans (Part C)
They will also include all other benefits not covered by Medicare. Whether or not the plan you choose includes dental services – for instance, routine checkups or cleanings – varies based on the plan you select. The amounts of monthly premiums, deductible payments, coinsurance payments, and copays depend on the plan you enrolled in. You will keep on receiving 100% coverage for the rest of the year after the plan pays you for exceeding the limit on out-of-pocket expenses over one year.
Medicare supplement insurance
Also referred to as Medigap, this is supplementary insurance, which pays out-of-pocket fare associated with Original Medicare. Medigap policy can be procured from a private insurance firm. Since all Medigap policies are government-regulated, they provide the same basic benefits, irrespective of the geographical location or the insurance carrier. Thus, the only distinction among the 10 types of plans offered by most states is their pricing. Dental care is not generally covered by Medigap policies.
Some people with limited income and resources may be eligible for Medicaid, a program jointly funded by the federal and state governments to provide assistance in covering medical costs that are generally not covered by Medicare. Each state maintains its own rules in determining who is eligible for Medicaid. Medicaid’s EPSDT rule requires that dental services be provided to all enrollees aged 21 and under. Although many Medicaid programs provide for emergency dental services, less than half of the states offer full coverage.
Other Medicare health plans
There exist three kinds of Medicare health plans that can assist in lowering your expenses. Each one has its own criteria and eligibility.
- Medicare-Medicaid plans. These plans, only available in certain states, help to coordinate the benefits entitled to you by Medicare and Medicaid.
- Special Needs Plans (SNP). Through SNP, you may qualify if you have a chronic or disabling condition, need long-term care, and have both Medicare and Medicaid. Please note that these plans are not offered in every state. Some SNPs may cover dental care benefits.
- Program of All-Inclusive Care for the Elderly (PACE). After joining PACE, a group of doctors and nursing staff will coordinate your care. This program will pay for anything that is covered by Medicare and Medicaid, plus anything that the health care team believes is necessary for your health, which would include dental care. To qualify for PACE, you must be at least 55 years old, meet your state’s criteria for needing nursing-home level of care, and reside in an area served by a PACE organization.
Understanding dental insurance plans
In-network vs. out-of-network dentists
A list of dentists enrolled with your dental insurance plan will be provided to you. These are termed in-network providers; the majority of dental insurance plans pay for care only if you visit a contracted, participating in-network dentist, orthodontist, or other oral health care specialist. A visit to the in-network provider generally means you incur the smallest amount of coinsurance.
Most PPO plans allow out-of-network providers, meaning you could seek treatment from this provider. The out-of-network providers are the ones that do not maintain contracts with any dental plans; however, if it is a PPO, it still allows you to consult out-of-network providers, but will reimburse only a minimal amount, as opposed to those who are within the network. Thus, if never covered by the insurance, an out-of-network provider will have you incur more costs.
However, the HMOs are usually restricted to in-network providers. They will not pay for any dental care except for that provided through an in-network provider. Therefore, unless you decide to see an in-network doctor, your HMO dental plan will not cover any treatment.
Likewise, the Medicare and Medicaid plans have some lists of dentists and other oral health practitioners who accept these plans. To compare providers in your area, you can visit Medicare.gov.
Predetermination of costs
Some plans require that you, together with your dentist, submit a treatment plan to the plan administrator for consideration before obtaining treatment or a procedure. The administrator would assess your eligibility, the eligibility time limit, services covered, your co-payment, and the maximum limitation. This is called predetermination. Some plans make it a mandatory process for treatments that exceed a certain amount in dollar value. Other names include preauthorization, precertification, pre-treatment review, or prior authorization.
Annual benefits limitations
To contain costs, your dental plan may limit benefits based on the number of procedures or dollar amount in a particular year. In most cases, these limitations will allow for adequate coverage. But knowing what and how much the plan allows, you and your dentist can therefore plan treatment that minimizes your out-of-pocket expenses and maximizes compensation from your benefit plan.
Peer review for dispute resolution
Most dental insurance plans have a peer review process to settle disputes between third parties, patients, and dentists, thereby avoiding many costly court cases. The idea behind peer review is to have a fair and equitable system, giving individual case consideration and a thorough review of records, treatment procedures, and results. Most disputes can be resolved tolerably for all parties.
What is dental coverage?
Full coverage dental insurance
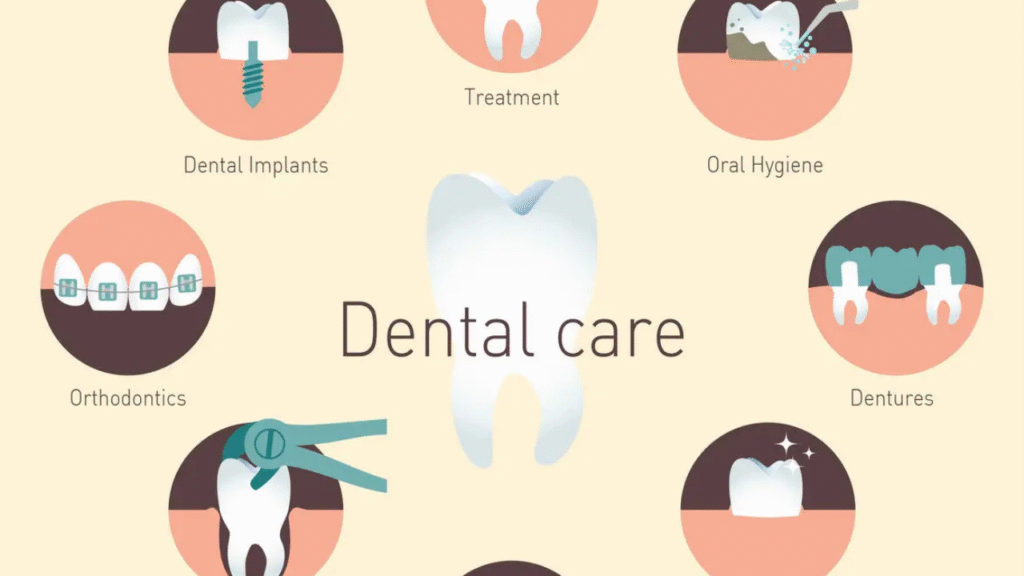
Full coverage dental insurance is another name for comprehensive dental insurance; it refers to insurance covering a fair bit of these categories of dental care:

- Preventive care: Dental experts recommend you have regular cleanings and checkups in order to maintain your oral health once every 6 months. Preventive care includes regular exams, cleanings, fluoride rinses, and oral cancer screenings. X-rays also fall under preventive care. This helps forestall dental issues from developing or catch such issues early before they get worse.
- Basic or restorative care: This means simple fillings, crowns, and tooth extractions, which are used to treat cavities, gingivitis, or any other form of oral infection. Usually, most dental plans provide coverage for X-rays relevant to these procedures.
- Major dental care: These can mostly be restorative under more complex and invasive procedures, often requiring anesthesia or oral surgery. Major dental care may cover:
- Endodontics or root canals.
- Periodontists the care of the structures that support and surround the tooth, including scaling, root planing, and management of acute infections or lesions.
- Prosthodontics, like dentures and bridges.
- Oral surgery for issues such as removing impacted wisdom teeth, tissue biopsy, or draining minor oral infections.
- Certain full-coverage dental insurance policies may even include dental implants.
- Orthodontic care: Some full-coverage dental plans will cover orthodontia like braces, retainers, or aligners, but usually only for children.
- In most cases, you are covered for two preventive visits per year. With an individual policy, you may not be able to access coverage for a year for periodontics and prosthodontics.
Most plans are arranged under the 100-80-50 structure. Accordingly, they pay 100% of the cost of preventive care, 80% for basic procedures, and 50% or a bigger co-payment for major procedures. But there may be some exceptions, such as not covering sealants at all.
Does dental insurance cover braces?
A very popular insurance question from all over the world is: Does the insurance cover braces and other sorts of teeth straightening? Any plan’s provisions for orthodontics-braces, retainers, and aligners usually require an addition for which you pay an extra fee. If you qualify for treatment of crooked teeth or malocclusion, you should read your plan’s details regarding investigational coverage of orthodontia. Most full-coverage dental plans cover orthodontics for children only.
Dental insurance limitations
The limitations of dental insurance coverages generally regulate how much reimbursement is paid on the various benefits permitted by a plan in a plan year. This is equally true for full-coverage dental plans.
Annual caps
Every plan has an annual cap on reimbursement in a given year. In many cases, this cap is rather low. Annual maximum reimbursement means your plan’s limit for all expenses in a year. Any expense borne beyond that limit is paid by you.
About half of the Dental PPOs pay annual maximums lower than $1,500. Based on the plan, with a maximum of $1,500, any of the treatment costs above this must be borne by you. Some patients requiring crowns, root canals, or oral surgery can quickly reach maximums. Usually, there is also a lifetime maximum for orthodontics.
Some plans may exclude certain services or treatments to lower their costs. You need to know what specific services the plan covers and excludes.

More Exclusions
Most dental insurance policies contain a variety of limitations and exclusions that allow them to not charge you more while keeping dentistry from becoming prohibitively costly. In fact, all plans exclude experimental procedures and services rendered, whether performed by or under the supervision of a dentist. Some exclusions can be a bit more subtle, however. In some cases, the benefits of dental coverage will overlap with those under medical health insurance. Read and learn about the terms of your dental insurance plan. Some exclusions in your dental plan may be covered by your medical insurance.
Dental Insurance and Timing
In addition to knowing what types of care are covered under your plan, you should be aware when coverage for each category of care becomes effective, as well as the frequency allowed for that type of care.
Period of waiting for dental insurance
Most often, you can indeed get almost all forms of preventive care without any waiting period associated with the coverage. Yet there is normally a waiting period before that type of care is covered by the plan: preventative, restorative, or some required oral surgery procedures.
Most policies cover only preventive and some restorative care, endodontics, and maybe a couple of surgical oral procedures for the first year. The waiting period is usually 3-6 months or even longer (up to 1 year), depending on your plan and the specific dentistry treatment. In such cases, you will have to use the policy for a little over a year before covering any treatment. Each orthodontic rider has its own separate waiting time.
Dental frequency visits for therapy
Generally, two visits a year are what most experts recommend for adults to go to their dentist. Company dental policies tend to subscribe to this idea, with different language. Your policy might read that it will pay for a preventive visit every 6 months (but not closer together) or may state that visits occur twice in a calendar year or twice in 12 months. Familiarize yourself with the policy, and you’ll know how to plan your visits.
Typically, these include but are not limited to time limitations on certain other services such as X-rays, fillings on the same tooth, crowns and bridges on the same tooth, or fluoride treatment for children. For example, your policy may reimburse a full series of X-rays only once every 3 years.
Dental insurance and limitations on pre-existing conditions
A maximum period for enrollment of 6 months is pretty common, and few dental plans allow coverage of conditions that existed before enrollment. You will need to pay for any continued treatment from your own pocket.
What You Should Do Before Getting Any Dental Services
Before any dental procedures, read your dental insurance policy thoroughly to see whether the procedure is covered. If in doubt, call your insurance company.
This is especially important for big procedures, because patients can ask their dentist for a pretreatment estimate. It allows the patient to know how much he will have to pay after any coinsurance, deductible, and policy maximum.
Before a dental procedure, check with your dentist and insurance company if you need any preauthorization, and if your dentist has obtained it. The preauthorization will confirm whether your dental procedure is covered by your plan and the corresponding amount that your plan is going to pay for it. Preauthorization can also validate whether you meet the timing requirements for the procedure, as many plans will not cover certain dental procedures unless preauthorization is received from the dentist.
It is also wise to be familiar with how your dental plan handles emergencies. Most have some provision for urgent care or after-hours care, but you may owe a deductible, a co-pay, or a larger percentage of costs.
Important Things to Think About Before Buying Dental Insurance
Buying dental coverage at work is probably the easiest since it tends to be cheaper than signing up for an outside policy. If you are getting a plan for yourself and already have a dentist, you can ask them for recommendations for particular insurance plans based on your dental history, as well as inform you if they are in network with a certain plan.
What to know before comparing plans
- Whether your dentist or any specialists you might need are in-network
- Total yearly plan costs, including premiums, co-pays, and deductibles
- Annual maximum
- Out-of-pocket limit, if any
- Restrictions with regard to preexisting conditions
- Coverage for braces, if needed or expected
- Emergency treatment coverage if in need of treatment while away from home
- Whether you can select your own dentist
- Who controls treatment decisions — you and your dentist, or the dental plan
- Whether the plan covers diagnostic, preventive, and emergency services, and to what extent
- Routine treatment covered
- Major dental care that is covered
- Possibility to see one whenever necessary and schedule appointments that fit their routine
- Who is covered under the plan, and the period when coverage goes into effect
You should also demand regular reviews on the level of premiums to ensure that the UCR or the schedule of allowance payments is equitable. This analysis will help your benefit levels be optimized to make sure that every dollar you spend is well utilized.
If you have their dental benefits plans, inform the administrator or carrier of your primary plan that you are dual-covered. Sometimes, there may be complete assurances as to the coverage one is entitled to, where benefits overlap and there is a benefit through the first plan for an exclusion by the second plan.
Opt for a plan that limits dollar or service benefits instead of excluding types of services. You can have the best care and be able to work with your dentist on treatment plans that can provide the most and highest-quality treatment.
Your dentist cannot answer questions about a specific question chord on insurance question or how much coverage a certain procedure will have. Every plan has different coverage for its beneficiaries according to the contracts negotiated. If there are questions regarding coverage, reach out to your employer benefits department, your plan, or the third-party payer of your health plan.
Takeaway
Just like health insurance, dental insurance does not have a one-size-fits-all approach. Knowing what types of plans and coverage are available can help you make the right decision about which option is best for you and your dental care. Always make sure to check any dental insurance you already have to get the coverage you need, at a price you can afford.
FAQs:
What does dental insurance in the USA usually cover?
Most dental insurance covers preventive care like cleanings, exams, and X-rays, plus partial coverage for basic and major procedures.
Are cosmetic dental procedures covered by insurance?
Generally, cosmetic procedures like teeth whitening or veneers are not covered, as they are considered elective and not medically necessary.
Does dental insurance cover orthodontic treatments like braces?
Some plans cover orthodontics, especially for children, but adult braces often require higher-tier plans or additional orthodontic coverage.
Are dental implants included in standard insurance plans?
Most basic dental insurance plans exclude implants. Some comprehensive or premium plans may cover part of implant procedures.
SamhithaHealth & Wellness Content Writer
a Health & Wellness Content Writer with over 6 years of experience creating research-based health articles. She specializes in nutrition, weight management, diabetes care, skin health, and healthy lifestyle practices. Here content is carefully written using trusted medical and scientific sources to ensure accuracy and clarity for readers.

